Podcast Debut: Glanda Tells All

Last September, a former radiation therapist named Cheryl Turner contacted me on Glanda’s Instagram and asked if I would be interested in being a guest on her Rad-Cast podcast. Rad-Cast is a radiation podcast available on all platforms that provides CE credit for radiation professionals, and as a former RT I knew that she knew the ins and outs of the field (literally).
First response… *looks around and behind me* “Who, me? Are you sure you got the right girl?” I am sooooo not the public speaking, center of attention type (and there was no way she could have known that) but my fingers typed “yes” and some other stuff and I hit send before I could talk myself out of it.
Uh oh. Now I was committed and the closer it got the more nervous I got. It’s not unusual for me to fumble my words or say something stupid and that’s all I could think about…making an idiot out of myself in this podcast that God knows how many people might listen to. But thankfully Cheryl sent me some potential questions ahead of time which allowed me to flesh out some of what I might say and make sure it was the kind of content she wanted. She was also more than patient with me in the scheduling and recording portion of it all, since I work full time at UAB and coach a university dance team here in town.
So we scheduled a time and date and after a full day of work and dance team practice, we set things up to do this thang (as we say in the south).
After an hour and a half or so, I emerged from my podcast lair back downstairs and K.T. asked how it went. Apparently I had given all my answers for the podcast because I really didn’t have an answer for him. I literally told him, “I have no idea. I just talked.”
But so I don’t stall any longer because I’m STILL nervous about the fact this happened, here’s my podcast debut…
When a Young Adult Gets Cancer: From Her Perspective
Enjoy, my friends! Onward and upward!
Professions of a Panelist

Last week, K.T. and I had the opportunity to sit on a patient panel with 4 others at the UAB Head and Neck Cancer Survivors Support Group meeting that I’ve been a part of for about a year or so. The questions prompted us to traipse back through the hard days of our journeys and dig down into the rawness of it all. The questions surrounded fear, mortality, diagnosis, and heartache among other topics, but even though I was there to share my story in order to potentially help others, I left feeling that I was the one that was helped instead.
The meeting started off with each of us introducing ourselves, including the UAB faculty and staff that so graciously give their time to be there as a resource to our patients. Several questions were then asked to the patients to kick off the panel portion, and then a question to the caretakers was posed. “What the most rewarding thing and the hardest thing you faced as a caretaker?…”
K.T. spoke up and described the delicate moments from when Dr. Carroll called to tell him that surgery went well but his wife of 2.5 years likely had cancer until the moment Dr Carroll told me himself. He took us through his emotions and the unimaginable task of breaking the news to my parents and his, who were all there waiting for me to come out of recovery. And he briefly touched on the decision he had to make to wait to let Dr. Carroll tell me the news when he did his rounds rather than him telling me and not being able to answer the questions I would inevitably have.
This wasn’t the first time I had heard this story. K.T. has shared these moments with me several times before, the first being surgery day. He had joined me in the hospital bed after everyone had gone home for the evening and he told me about all I missed while I took my very long surgical nap. But at each different point in this journey that I hear him describe those long, grueling moments of that day, another layer is exposed and I learn something about life.
For the first time this week, I feel like I truly grasped the weight that K.T. has had to bear for me and with me through all of this (which all of the sudden seemed heavier to me than actually having the cancer myself because it’s not just his own load he’s carrying). He’s had to carry parts of mine too. We’ve had countless conversations where I’ve apologized for what we’ve gone through with my health, and I’ve spent hours praying that he hasn’t built up resentment towards me for all the slack he’s had to take up while I’ve recovered and adjusted to a new normal, physically and emotionally. Deep down I know he hasn’t because that’s not his heart, but this realization of the heavy load he’s been gracefully carrying was an important one for me.
But what does this realization have to do with any of you? And why even share this kind of thing? Because there is absolutely an essential balance between being concerned with what is going on inside of you and understanding that your close friends and family are experiencing a battle of their own alongside your diagnosis that they weren’t expecting either.
For most people going through a tough health issue, it’s hard to see past the hard days that inevitably come more often than you wish they did. It’s hard to see past the emotional torment you’ve fought through because you didn’t have any control over the physical that caused it. And it’s hard to look in the mirror and not totally recognize the person and the differences that have also happened because they had to. But your family and your close friends have the same basic human need to be understood, just the same as you do.
When the days are hard for you, they may feel guilty that they can’t offer you more help to ease your pain. When your emotions and thoughts are all over the place and unpredictable they may feel like they fall short of knowing what to say to comfort you. And when you look in the mirror and feel insecure about what you see, they may wish they could fix it or boost your confidence. But the truth of the matter is they can’t.
Now this is by no means meant to make you or anyone else feel guilty. You are not selfish for thinking and feeling the things you do. These are all very normal things that happen in the process of healing on both sides. But the key here is understanding its a process and that requires forward movement. Getting stuck in a rut isn’t fruitful for you or the people who love you. So in and effort to keep myself honest and share my story with you as I’ve promised to do, I have to encourage you to lift your eyes and try to see things from a different perspective and keep bettering yourself.
Ask yourself these few questions:
- Am I complaining too much?
- Blaming too much on cancer?
- Am I making excuses for my behavior because of what I’ve been through?
- Have I picked up the load that I’m capable of, now that I’m past things a little?
- Am I doing my best to live a life that makes me proud and pleases the Lord?
Those are hard questions, and I have just as much personal identification and work to do within myself as the next guy, but cancer or not, being honest with ourselves and giving life our best each and every day is worth it.
Now, I hope it doesn’t take a patient panel or a story you’ve heard several time to awaken your spirit from the famous fog that cancer brings into our headspace, but I hope and pray you lift your head and take another step towards your new normal and the BEST normal that the Lord has waiting for you!
Treatment’s Over…What now?

This period, often called “the lull” is BY FAR the hardest period of time you will experience in comparison to all the others. It’s the time immediately following treatment, and for most, it’s the first time that you are without any kind of active treatment. From the outside perspective, this time would seem to feel the best and provide some much needed relief. You’re finally free from being zapped every day and/or having poison pumped through your veins, but freedom is unfortunately not really the reality that comes with this period of time.
I remember just one short week after my last fraction of radiation, I was gently massaging my skin and neck while sitting at my desk and thought I felt a hard spot around where Glanda used to be. So I set off to find Dr. Spencer in the hallway as soon as I could to ask her to do a quick feel to make sure I wasn’t losing my mind. (Perks of working in the department that treated you I guess). Turns out, I wasn’t wrong. There was absolutely palpable hardness, but it wasn’t disease. It was simply induration, or stiffness caused by scar tissue and all the radiation I had just received, something that’s super normal after everything that side of my head had been through.
No active treatment to a cancer patient means thoughts of heightened risk for the potential new growth or recurrence. It means fixating on the fact that essentially nothing is being done to kill your cancer anymore (if any still remains) and that’s some scary junk. To add to that, there’s a good chance you’re emotionally and mentally SPENT right after treatment so fending off these thoughts is hard and taxing on your body and spirit.
Since treatment, I’ve learned to poke around on things a little less. I still massage and stretch my neck like a good little patient, but I try to do it mindlessly and focus my thoughts on how far I’ve come in my healing and ability rather than what every little thing I’m feeling is or might be.
But what can you do as you tread the waters of this weird stage of the journey? Well, what you can’t do is go back into treatment (and we all know that’s not actually what we want) but there are a few “normal” things you can do that I believe help. But honestly recognizing this season for what it is, is half the battle.
Eat
Don’t roll your eyes at me! I know this sounds dumb and like an obvious answer to…well, life. But treatment takes a lot out of you, including your appetite, your taste, and in some cases your ability to eat. So the time after treatment is a great time to start working on building your strength back. Start back eating if you can (or continue to eat) foods that are rich in protein. Those are the foods that re-build healthy cells and will fill you up the most. It’s also essential to find foods that taste good to you and eat a lot of those to build your caloric intake back up until you get closer to more of where you used to be. Most importantly, remember this isn’t going to happen overnight. It’s a marathon rather than a sprint.
Rest
Sleep, like protein, restores your body and gives it the time it needs to repair itself from the damage that was caused during your treatment. While not everything will heal up perfectly and return to what it used to be, sleep is still extra important because our bodies do have amazing healing ability and giving your body what it needs aids in your overall wellbeing and quality of life. So this is the time to sleep, take a nap, relax on the couch, sleep some more, dream about your favorite things, take another nap, watch a movie, nap again, and then finally go to bed to prepare for the next day. And besides, sleep is probably all you’ll feel like doing for a while anyway. So why not take advantage of a good rainy day, a few good movies, and all the zzzz’s.
Take a walk
Around about a week or two post-treatment, it’s important to make sure you’re spending a bit of time during the day moving around and gaining some muscular strength back as well. I know I just suggested a lot of sleep, but there’s a balance in there somewhere. You don’t want your muscles to atrophy too much if you’re able to get up and move around, but you also don’t want to overdo it too soon. Maybe this means moving from the bed to the couch a few times a day. Maybe it means getting up and getting a shower. Or maybe it means going for a walk or running a few errands around town. Just take it easy and do what you feel like doing. Movement is also an excellent idea if you are at risk for lymphedema (swelling because of the buildup of lymphatic fluid). It really depends on the person and the severity of treatment side effects, but the sooner you get back to doing more normal things, the more normal you might start to feel overall.
Reflect
I’m not sure how this will resonate with everyone else, but working to accept and understand what I’ve been through proved to be very healthy for me. This doesn’t mean I figured out the “why,” though. Cancer doesn’t give a reason when it arrives. It just shows up, so save yourself some trouble and forget every trying to find the why. (I wish someone had told me sooner). When I suggest trying to understand what you’ve been through, I mean understand that what you’re going through is a necessary byproduct of something you have no control over and that’s ok.
Writing my experiences down, talking to someone I trust, or just quietly pondering things all healed me bit by bit but as always, it’s crucial you keep your thoughts in check and not let them get out of hand. The truth of the matter is, what happened happened and it must be processed. There will inevitably be some pretty dark days following treatment and throughout this journey overall, and everyone will manage those differently. But don’t just step foot out of the treatment room and forget where you came from. Your journey wasn’t for nothing and you’ve made it! That’s a really big deal!
Overall, the goal post-treatment is relatively simple, however not simple to do. Find some sort of normalcy and routine. Now, I 100% understand that’s a bit of a joke because NOTHING feels normal after treatment. Nothing. But set some version of normal as your goal and go after it day by day. Before you know it, you will be looking back at the post-treatment days admiring how far you’ve come and you might even recognize a few pieces of normal in there too.
Onward and Upward

At each phase of this journey, I have had to remind myself to look back at where I’ve been so I can better focus on where I’m headed. Glanda has been known to say “onward and upward,” and that makes a polite nod to the fact that you’re coming from somewhere and you have greater places to go.
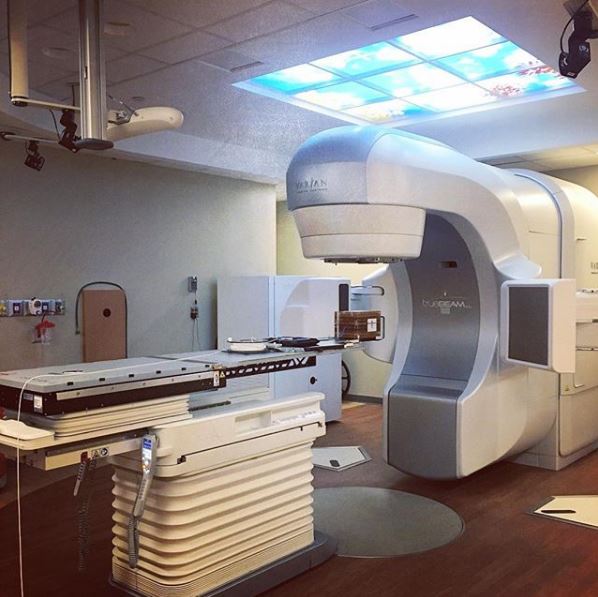
As I left work down the long treatment hallway on Tuesday night, I stopped and peered into the vault where I was treated just a year and a half ago. On a normal day, I don’t dare stop, but instead walk as fast as I can down that hallway to ignore the usual treatment noises and bustling that happens around that area. But tonight, the Varian Truebeam STx sat there quietly “sleeping” and looked so peaceful that it struck me some kind of way and I had to stop and stare.
What? Am I crazy for personifying the radiation treatment machine that made my skin look like the walking dead? Probably, but the longer I move away from the hardest days of my life into days where the fruits are starting to grow from the seeds of faith that were planted then, the more I begin to have a strange fondness for the things that healed me and helped me along. And the machine is just one of those things.
I’ve honestly gone through a period of time lately where I didn’t know if I still had purpose in the UAB Department of Radiation Oncology. I wasn’t clear on whether it was time for me to move on or not, and I definitely wasn’t clear on if it was time, then what would that even look like? Have I been here long enough that my story doesn’t resonate with anyone anymore? Is my story too specific that it doesn’t reach enough of our patient population to matter? Am I done here trying to make an impact on our sweet patients that have come behind me and face the same kind of hard days of knowing yet another treatment was coming?
The short answer to that is no, and it’s moments like Tuesday night that remind me of that. This place is without a doubt the place that broke me and put me back together, but now that those things are long gone, it’s what I GET to do.
Last weekend, I got to go to my 2nd annual ROAR gala (as a volunteer) where hundreds of people gathered in formal attire to raise money for cancer research in the Department of Radiation Oncology through a silent auction as well as a live auction. Last year, I was 3 months out from treatment, quite emotional watching the whole thing go down as a survivor (don’t worry, I wasn’t crying in public) and my arms had just recently started losing sensation. This year, I walked in proudly and excited (also awkwardly by myself since K.T. was out of town) to see all that would be done financially in honor of those that will need radiation treatment in the future. The numbers aren’t in yet, but a Maserati was auctioned off…it’s A LOT.

In a few short weeks, I will be transitioning out of Regulatory Compliance for clinical trials into a role much more suited to my skills. A chance to create publications for our department, a chance to plan departmental events, and a chance to improve the educational documents that our patients receive before, during, and after treatment among other things.
In the same few weeks, a podcast I recorded with Rad-Cast in February will air where I get to talk about my experience as a patient, how my job/coworkers influenced that, and how faith guided me along the way.
And in another few weeks, I get to sit on a panel with other head and neck survivors and speak to an audience of other head and neck survivors about facing fear and overcoming the struggles that come with cancer.
And ALL of these things are things that fell in my lap because of what I’ve been through. People still look at me like I’m insane when I say that “cancer has been my biggest blessing,” as they probably should, but, y’all look at God! I surely didn’t do any of this on my own and without cancer, none of these things (including moments to stare at that terrifying STx machine) would have been part of my life. Do I want to do it again? HECK. NO. But most of the time, I’m kind of glad I did. (That still makes me a little nauseous to say.)
So with my bit of reflection from the other night, I thought now would be a good time to share a little visual journey of where I’ve been so I (we) can continue to focus on where we’re going!
Onward and upward!




Tips for Choosing Your Oncologists
Choosing the team of physicians that will care for you during your treatments and follow-up can be a hard decision. You are likely still processing your diagnosis at the time you will need to make this decision, but there a few things you might consider that could make the choice a little bit easier.
Do they make you feel secure?
Security is a big deal in cancer treatments. Vulnerability tends to increase during this time so you want to make sure the person that you’re trusting your life and overall well-being with is someone that is going to be responsive to that and treat the situation with the delicacy that it deserves.
When you attend your oncology appointments it’s important to feel safe, protected, and generally heard and answered. There are a million oncologists out there that will be able to quote statistics and most-recent research findings, but if they don’t create an atmosphere that allows you to be open and honest with them, then they might not be for you.
Many people feel like if their doctor gets them healthy then that’s all that matters, but hear me when I say that you need someone that meets your mental and emotional needs as well through this journey. They are not counsellors, but their answers need to be ones that you trust and that you are comfortable with. And if they don’t have the answers to questions you’ve asked or symptoms you’ve presented with, they need to be diligent enough to send you to someone who will.
Are they willing to spend time with you?
When I look back on my care team and what meant the most to me, it’s time. 100%, without a doubt, time. The people that took the time to listen to me, to try and understand me, and to try and connect with what I was feeling on some level are the people I truly felt like cared about what I was going through and truly cared about seeing me get better. Of course, as a patient you want to respect the fact that your doctors have other patients to see, but pay attention to their mannerisms and body language.
Do they come in and seem relaxed or do they seem rushed? Do they take a seat and physically get on your same eye level or do they stand by the door for most of the appointment? Do they seem truly familiar with your case or are you having to remind them of the details? Do they take their time in listening to what you are struggling with or do they brush it off like you’re making things up or it’s not as bad as it seems?
All of these things are crucial and I do acknowledge that everyone’s needs are different, but the feeling of actually being cared for is the generally same across the board.
Do you know other patients that have been treated under their care?
We all know the power of a personal recommendation. Whether it’s which grocery store to shop at, which hair salon to visit, where to shop for clothes, or the best restaurants in town, people talk about the things, places, and people that they have had a good experience with.
With cancer care, it’s not much different. Patients will talk about their doctors that helped them feel better and, even moreso if they helped them feel better quickly. To no surprise, cancer patients that undergo treatment also tend to develop a certain fondness for their care team because they feel like these are the people that “saved their lives,” so make sure to ask specific questions to see if you agree with how they were managed as patients and read between the lines.
Are they good at what they do?
This one probably seems like a no-brainer and I realize many of these suggestions involve feelings rather than expertise, but bottom line is that it all matters. Before considering a particular physician for your oncology care, take the time to do your homework. Read reviews about their achievements, their educational background, their honors and awards. Are they affiliated with specialized organizations for their field? Do they participate in grants and research? Have they published any papers?(PubMed is a great resource) I could go on, but you get the point. Credentials matter!
Physicians are wonderfully brilliant people on our earth, and I’ll be the first to argue that the majority of physicians go into the profession to care for people with their hearts as well as their souls. But for some it’s all too easy for patients to become charts and numbers when clinic schedules are jammed packed and days are long. And that’s just the facts, unfortunately.
Working in the field, experiencing cancer myself, and also having various family members need oncology care has shown me all sides of the field, so I share this with you to encourage you and empower you to look for the BEST oncologists out there. Look for the ones that provide what YOU need. Every patient is different and will have different needs in each of these areas. I just pray that these few insights above may lead you to think about things differently as you go to make the decision about who will care for you.
I Cross My Heart

Because it’s Valentine’s Day and everyone is talking about LOVE, Glanda wanted to get in on the fun too, but while you’re probably already rolling your eyes because Valentine’s Day is kind of dumb and love is a little mushy sometimes, don’t give up on reading just yet. There’s a point!

K.T. and I met in 2012 in a church small group for young professionals. We started dating November of 2013 and we were married March of 2015. And in the 4 short years we’ve been married, we’ve faced my mom’s breast cancer diagnosis and treatment, the death of 3 special family pets, the loss of two different jobs (both mine), my diagnosis and treatment, and my rather steep climb back to physical and mental health. My poor husband truly had NO idea what he was getting into when he stood toe-to-toe with me and said “I do” on that brisk March evening.

At our reception, we kicked things off with our first dance to George Strait’s, “I Cross My Heart,” sung by my longtime friend Ryan Kinder. We had picked the song for the lyrics of course but also because I had memories of listening to it in the car with my mom when I was a little girl. K.T. and I held one another closely while we spun around the room and giggled about all the things that had happened so far on our perfect day and we giggled out of nervousness for what was to come later that night… (I can say that, right?)
This past Christmas as we were making the short 45 minute drive from his parents’ to my parents’ house, we listened to a few George songs with excitment knowing my dad had a Las Vegas surprise to take my mom to see George Strait under the tree. *See bottom of post for more details.
We shuffled through a few classics and then “I Cross My Heart” started playing. K.T. grabbed my hand sweetly as we sang along and remembered that sweet day we got married. Then the bridge came…
“And if along the way we find a day it starts to storm,
You’ve got the promise of my love to keep you warm.”
Next thing I knew, I was a blubbering, crying idiot. When you get married, there’s an understanding that you will face hard times, but never, ever do you think it will actually happen to you. In all my days before March 28, 2015 (and really up until diagnosis) I never thought I would put my husband through the hardship of caring for his cancer patient wife just 2.5 years in. It felt like the worst kind of “storm” short of death that I could imagine, but K.T. kept his promise and always kept me “warm.”
He bathed me after surgery when I could barely even make it into the shower by myself, he made fast food runs knowing that I might not even want to eat what he came back with anymore when he got home, he waited on me hand and foot, and he’s never missed a single day in telling me I’m lovely and beautiful. He’s never made me feel bad about having to care for me. He’s never cried because I was sick…only because of the blessing that I was getting better, and he’s never been anything but thankful for the journey the Lord has had us on. Yeah…I don’t deserve him.
But while I will unapollegetically share with you the man and true blessing my K.T. is, I also want to stress something else very important!
It is crucial that you find and cling to people around you during your journey to love you, support you, encourage you, validate your feelings, and be selflessly willing to help you!
So I’ve put together a short list of things that I feel made my heart swell the most and filled up my love bucket as we’ve traversed some rough waters.
Hug people
No, I don’t mean strangers…unless you’re into that kind of thing (but they probably aren’t, so don’t do it). But take time to hug your people, your pets, your stuffed animals. Whatever. There’s this saying out there that 10 hugs a day improves your health. I don’t know how scientifically proven that is, but I’m willing to test it out. And I’m lucky enough to have a person, a pet, and a stuffed animal. Don’t judge me.
Can I confess that this was a hard one for me? I’m not a super touchy-feely person. I didn’t snuggle a whole bunch growing up (unless I have amnesia) and so when I got married and my husband followed me around wanting hugs and snuggles all the time in the middle of cleaning, laundry, or whatever else I was focused on…uhhh…I was really confused and used to turn around and stare at him like he was insane. But y’all, HUGS give me LIFE these days and I’ve tried to be better at making moments for them. Stressed out? Hug it out. Bad day? Hug it away. It’s become much more of my default, but I do admittedly still get a little annoyed when K.T. unplugs the vacuum to come steal a hug. But don’t worry, he always plugs it back in afterwards.
Take the time
I probably harp on this one a little too much, but don’t be too closed off or too embarassed to talk about what you’re feeling throughout life. And on the other side of things, don’t be too busy to listen. There are few things more important than connecting with someone on an emotional level. A level where you can relate and potentially feel some of the same things they are going through out of empathy. Look people in the eyes and share a little about your heart. People don’t always need advice or an action plan. Mostly, people just need a gentle understanding and maybe a hug or 12 (see previous point).
Our hearts are what make us who we are (fine, it’s actually part of our brains but I’m not a doctor so I’m going with heart), and it’s the moments of connection that create the memories that make a mark on others. It’s been said that it’s not always what people do for us, but how they made us feel. Don’t be scared to feel, yall. It’s magically freeing.
Say “I love you”
I love you is one of the most important things to hear for all ages, but don’t be deceived by thinking “I love you” is just for lovers. Feeling love and even expressing a love you have for something or someone can do wonders for your attitude (and attitude is everything in cancer. Trust me.) Love takes you to a happy place and focuses your thoughts on things that satisfy your soul.
Feeling awkward about it? Didn’t grow up in a loving family? I get it. But try working your way up to expressing how much you care for your people, whether it’s your friends, your family, or your spouse. I promise you that it matters more than you think.
See? That wasn’t too mushy, right? Just enough love to make your Valentine’s Day extra lovely. Happy Valetine’s Day, my friends.
Onward and upward!
*One of the main reasons K.T. and I were so excited about Mom and Dad’s trip to vegas was because we knew this is how she was going to find out. Dad had asked me to help him come up with a way to tell Mom so I waved my magic Photoshop/InDesign wand and came up with this. Glanda fam…meet Dad Strait! Yes, that is my father’s head on George Strait’s body.

Not What I Used To Be

Getting back to “normal” after diagnosis and treatment is a valued status that everyone faced with diagnosis yearns for. There are days of wishing you could rewind and other days where you feel like a total boss for getting through the emotional and physical stress and torment your body has withstood. And while life will never be the same normal as it used to be, sometimes it’s so far from how it used to feel that calling it “normal” feels fake and more like a joke. But fake or not, there’s still some kind of normal that we must live in each and every day as survivors.
Since I was a little girl, dance has been part of my life. It’s my normal. And while that will sound silly to many of you, dance was truly my constant during the many stages of development and learning on the way to becoming an adult, and actually since I became an adult as well. It was the place I escaped into when teenage life was too melodramatic or college stress became too much to bear. It’s the first thing I got back to after surgery, and the thing I was far too weak to do for months after treatment. It’s always been something that allows me to reach depths of my soul that I don’t know how to otherwise, and it connects me to music in this magical way to where I feel the melodies and lyrics in my bones. It’s special and always will be.
In April 2018, (6 months post-treatment) I was asked to take on the title Coach Val for the Samford University Dance Team. It was an easy yes, but it also came with a lot of doubt and literally zero confidence in myself to get the job done like I envisioned it should be. I love dance with all my guts, but I’d never taught a class and I suck at choreography. However, the Lord clearly saw me fit for the job or it wouldn’t have landed in my lap as it did, so I accepted.
Through band camp, two field shows during football season , Christmas break, and halfway through basketball season, we’ve made it. But Coach Val has had more moments of frustration with my body and ability than I can count. It has nothing to do with entering another decade of life this year either. It’s cancer and it’s radiation treatment, the gift that inevitably keeps on giving.
These days I fight through daily neck stiffness, very careful sleeping so I don’t wake up with a headache from a simple crick in my neck, arm and hand neuropathy from inflammation in my spinal cord, and overall lack of endurance and muscle strength that radiation robbed me of. I have to stretch the left side of my neck every morning and I have to treat my head like it might actually snap off if I’m not gentle enough.
But…
Coach Val has 9 college beauties that depend on me to be there for them, teach them, grow them, and help them grow the dance team program as a whole. I have 9 girls that are likely looking for the same deep connections again that they had in their younger years and 9 girls that are likely desperate to find those feelings again in a new season of life. So, I do my best to ignore my “new normal” and waltz back into the life that made me the woman I am. I do my best to tap into the strength only the Lord can provide, and I do my best to continue to grow in my leadership and other skills that might enhance my girls’ lives. And I’m not going to pretend it’s easy.
I haven’t truly danced from my heart since treatment, but it finally happened this weekend. As I hobbled into the house and embraced my husband in near tears, all I could say was “I’m just not what I used to be anymore.”
I was physically exhausted. My muscles were dead, the numb sensation in my arms and hands felt amplified as it usually does when I get hot and anxious, and my neck just felt fragile. Was I physically just fine? Yep. But the emotions are what sock me in the stomach the hardest. It’s when the “whys” resurface and the longing for a “rewind” button get to me, that I break and need picking up again.
Y’all, I don’t say it often, because I am wholeheartedly thankful for this journey and what it’s taught me, but goodness, cancer changes you big time.
I like to think I’m better for being a cancer survivor. And somedays I am. But other days I fail miserably at being a decent human. I like to think eventually it will make me a better wife, a better mom, friend, and coach after more of the dust settles and we get a little further out from treatment.
But the truest thing of all that applies to every aspect of my life is I’m simply not like I used to be. Sure, no one stays the same, but this wasn’t gradual. And I didn’t ask for this.
But it’s my normal now and today (and hopefully tomorrow too) I’m going to choose to be ok with that.
Cancer is Confusing

There are things about cancer that only cancer patients comprehend and fully understand. And because of that, there are things about cancer that us surviviors wish you knew.
Cancer is something I felt to the aboslute depths of my bones and it has recently become somewhat of a distant memory for me. If I’m honest with myself, I’ve intentionally blocked a lot of it out, and I truly never, ever thought I might feel a certain way about cancer being a distant memory. But I’ve found myself almost longing to understand why and what it is exactly that cancer has done to me as a wife, friend, daughter, and sister and I’m desperate to maintain the intensity of life and love it stirred up in my soul.
The further I move away from my cancer journey and that special hell I survived, it has started to seem less real at times. That’s a good thing right? Ehhh kind of. I don’t EVER want to relive what I went through. Ever. But I also don’t want to forget what it felt like, what it taught me, and the depths of emotion and compassion that I’ve found for those facing the same thing.
Most of the time I feel like I walked away from cancer with a fierce passion for living and understanding people and what makes them who they are. I’ve mended bridges with people I never dreamed to before cancer and these days, I tend to say things that I might not have said before cancer, both good, bad, and somewhat inappropriate and I’m good with that. Other times I feel like I lost parts of me that people relied on as steady constants and parts that helped them feel secure about my life on earth, and I don’t like it.
In processing where I stand in my journey now that the get-well, healing phase is pretty much over, there are bits of my heart that need sharing. Parts that have frustrated me, parts that have satisfied me, and parts that I just need you to try and understand. The things I wish I could look you all in the eyes and say.
So, here goes…
- I’m still the same Valerie
Acceptance is something I struggle with a good bit (just ask my husband how many conversations we’ve had on that topic), and this phase of the journey has been particularly hard for me. Whether it’s how many page views I get on this blog, how many people actually care to read what I write, how many followers I have on my related social media accounts, or how many people have chosen to take themselves out of my life for whatever reason, I’ve realized that people view you different during/after diagnosis than before when you were “normal.”
Yesterday evening, I attended UAB’s Head and Neck Survivor Support group we put on every other month. Pastor Malcolm Marler from pastoral care was the featured guest and one of the questions he asked us about acceptance and what that meant to us. Several of the other survivors spoke about what it took for them to find acceptance of the journey they’re on, but for me (being the youngest in the room by a longshot) the question struck me as more about the acceptance I feel from people now that I’m a “survivor.”
It’s true that I’ve found that some people are less understanding and accepting when it comes to seeing their friends in a different state than they’re used to seeing them in (and I’m not saying this is a conscious thought). It’s a situation that potentially makes them realize their own mortality, which was one of the hardest parts for me. At some point in all of our lives we will pass away. It’s a natural part of life but if you’re anything like me, I was happy assuming that I was going to live to be 80+ and just die of old age someday. And that’s still a pretty real possibility by the way. I indeed had cancer in my body, but that doesn’t mean I’m stepping foot into heaven any faster than anyone else. I’m still the same ole goofy, sarcastic, and ridiculous Valerie. I just had a different, slightly scarier detour to traverse than some.
- I didn’t choose this journey (and God didn’t either)
The more I learn about cancer and the perceptions that people have about it (general public as well as medical professionals) the more I want to wear a sign pimped out with flashing lights and my entire diagnosis and heart on it.
Someone once told me to “never try and understand cancer. It’s impossible.” And I still think those are wise words, but everyone tries. The instinct when a diagnosis comes is to figure out why and what you could have done to prevent it. I wanted to Google everything and figure out what my chances were and what might be coming, but Google simply isn’t God and doesn’t know (and thankfully my husband stopped me). Google is for sure a useful tool, but it’s one packed full of information and very little knowledge. It especially doesn’t know about my particular case, so I quickly learned that fighting my instincts and ditching the need for a “why” and relying on prayer and the plan that the Lord has for me, is a far better use of brain power.
There are a few things I do understand though. First of all, the Lord didn’t plan cancer for me, but it was never a surprise to Him. Was I mad at Him for a while that I had to go through it? A million times yes, but I Would. Not. Have. Made. It without His provision, His love when I was unlovable, and His absolute strength and mercy on my heart.
Secondly, I have strong feelings in my heart that this journey was given to me to bless others in some way that may be facing similar paths or others that have already been through cancer and haven’t dealth with the emotional side of it all yet. It’s why I continue to write words that may or may not be read. And it’s why I try my best to provide perspective and relateable words.
Lastly, my cancer wasn’t caused by anything specific. I don’t have HPV (human papillomavirus), I’ve never smoked, I’ve never been drunk (however I do enjoy a drink on occasion), and I live an extraordinarily lame life to be honest. It’s true I have a genetic mutation in my gene line, but there’s no solid proof that caused anything either. What’s the cause really matter anyway? The fact I had to go through it wouldn’t have miraculously disappeared just because I figured out why.
- I don’t need you to feel sorry for me. I need your compassion.
It is, indeed, saddening and often devasting when someone we know and love is diagnosed with cancer. There are moments in those times to cry, to mourn certain things (not necessarily the person), and times to lend a hand or heart and let them know you’re there for them and you care. Those needs are real and crucial. Alone is not a place you want to be through cancer.
When someone earns the title survivor after patient, the journey doesn’t end. They may have fewer doctors appointments, look healthier (or even like nothing happened), but fear of recurrence will always be real and scars and various other reminders will always be there to remind us that life got really scary at one point. This is why I will unapologetically tell you to ask how your friends and family are doing and not be scared of the hard answer they might give you.
Ask them about the hard times. Ask them about the ways life is still hard or what’s scary about the future still. There are plenty of people that won’t want to talk but it’s actually kind of therapeutic to talk about it. Most of all, just be a friend and listen. No one expects you to have answers or wisdom about whatever they tell you. They likely just need that feeling of understanding and acceptance…simple compassion.
So, cancer is confusing. Some days are still hard, even if it’s less than it used to be. Be a friend. Give grace. And be open.
Onward and upward.
The Appointment Process

After diagnosis, it’s hard to parse through the feelings of fog and fear and focus on what’s next. And honestly, sometimes you don’t even feel like thinking about what’s next, much less focusing on it. Treatment options will vary from case to case, but knowing the plan is comforting for some and, in my opinion, the more you know about how to care for yourself (or your loved one) during these times, the better. (PSA: I do NOT advise looking to Google for anything because I’ve done it and it’s miserable.)
Consultation
Your radiation consultation appointment will likely be sort of a recap of many of the things you already know, but it’s very important. Your radiation oncologist will review your recent health history, pathology, and possibly some prognosis details. They will also talk through your treatment options with you and let you know some of what to expect. This is a great appointment to ask questions that have come to mind since initial diagnosis. Your radiation oncologist will explain the treatment process with you and let you know how many treatments you have ahead of you.
Depending on your particular cancer, you may have a few “homework assignments” to complete before you come back for treatment also. For me since I was head and neck, I had to have a dental exam to make sure my teeth were healthy enough to endure radiation, and I also had to have a mouth piece made that I would wear during treatment.
Otherwise this appointment is one of the easier ones. It’s a sit and listen, ask a few questions type situation. Nothing scary so far.
Simulation
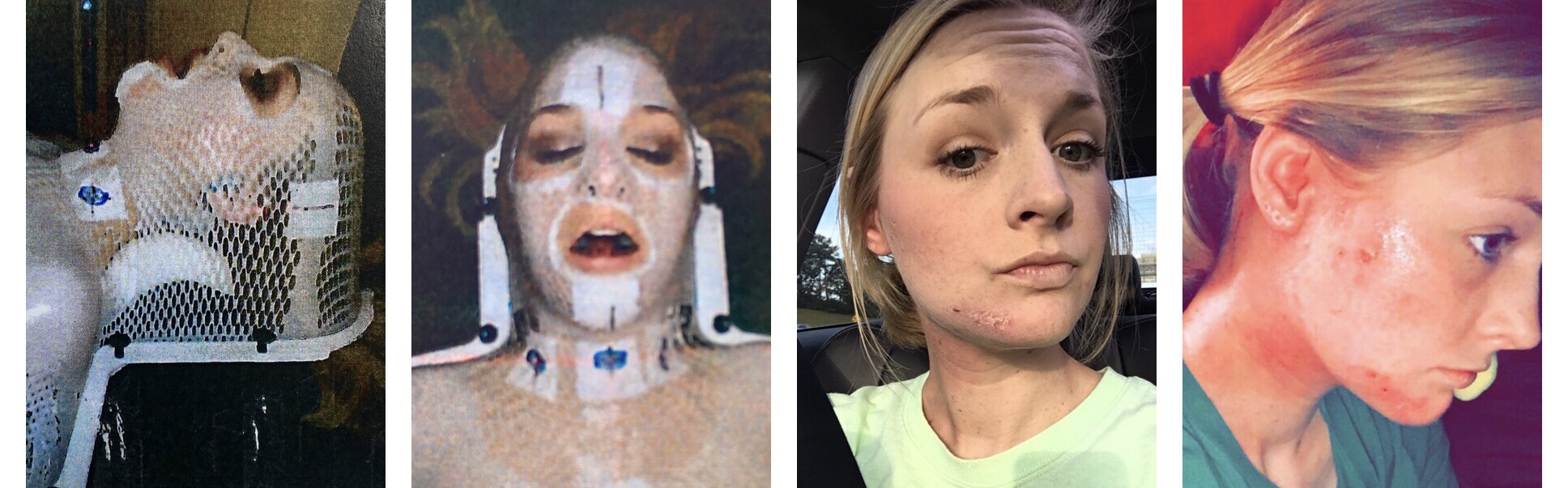
Simulation is a bit scary…or least that was my experience for various reasons. It all just became VERY real to me right then that I was, in fact, about to have cancer treatment. I work in radiation oncology, but somehow I had escaped seeing one of these crazy immobilization maks or if I had seen one I didn’t remember or didn’t know what it was. Regardless it happened and I survived it with somewhat minimal tears and it was on to the next.
From what I know, it is relatively common to have some sort of form made that your therapist will use to get you setup in the correct position each treatment, but not every disease site requires this.
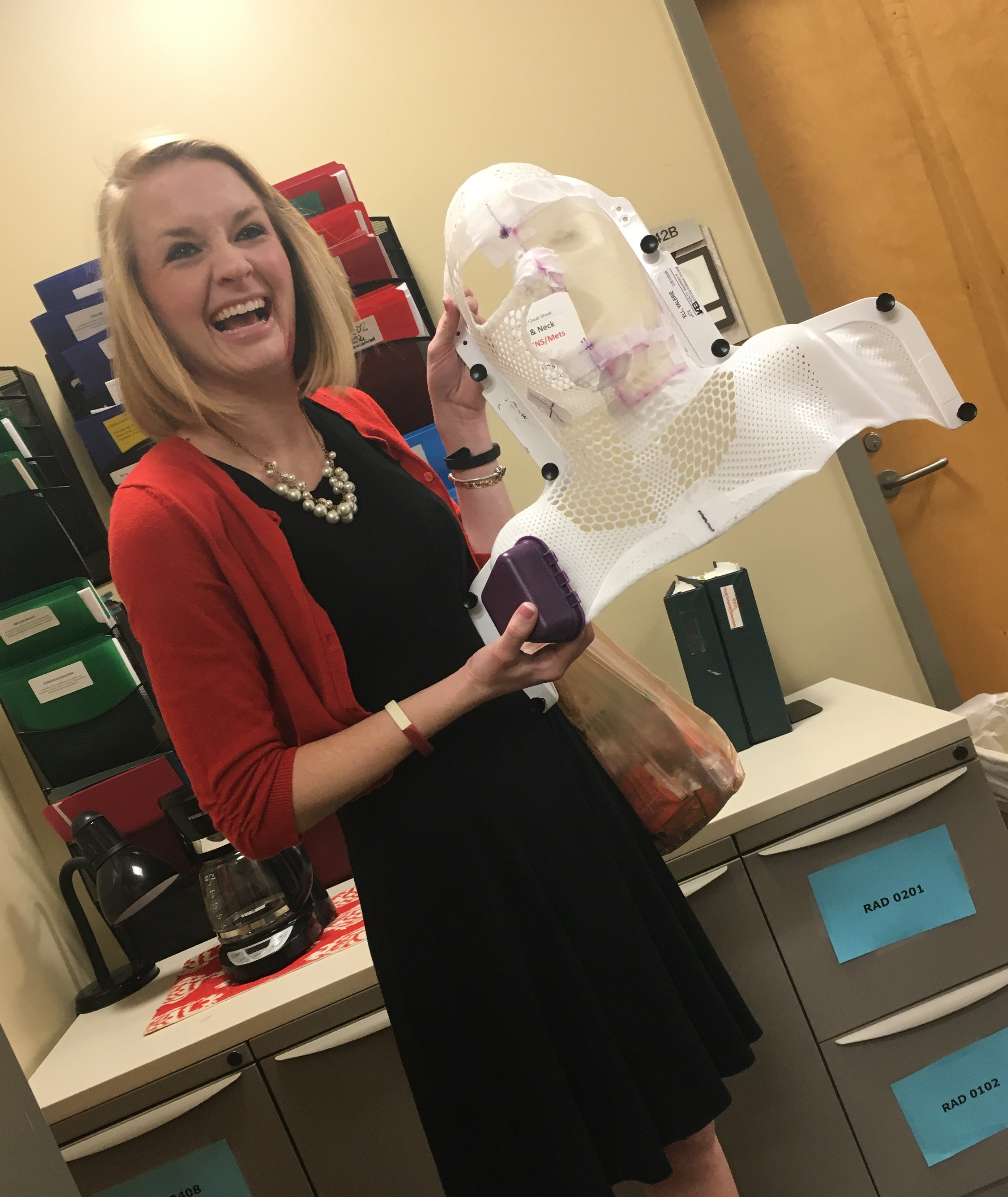
For my simulation, they laid me back on a table similar to a treatment table. They showed me the mask materials beforehand and explained everything to me as much as they could. The mask in its original form is completely flat. It looked like a hard plastic, person-shaped frame with a net-looking flimsier plastic in the space between. The plastic would be heated up in order to make the material more malleable and it would then be placed across my face and buttoned down to the table until it cooled off and hardened. I could see fine, breathe fine, and could hear fine so I knew I was fine but that didn’t scare me any less. This process didn’t take long but hearing the snaps click into place and knowing you had to hold still underneath plastic was a little nervy…and I soon realized that I would have a similar experience each and every treatment.
But I don’t say any of that to scare you. Each person has a different experience. And not everyone gets a mask. I tell you because no one ever told me and going back to my previous statement, the more you know the better you might handle things.
The rest of the simulation appointment involved a quick CT scan with contrast and a few marked stickers to also help with treatment alignment. Consider the simulation as the dress rehearsal of it all…but don’t worry, you don’t have to perform in the days to come.
Treatment

Treatment itself was relatively simple. I would change into my gown, head to the machine, get situated with my mouth piece, warm blanket (sometimes), and my mask. At that point my therapists would exit the vault and move to their station where they could see me, talk to me, hear me, and work the machines. From that point on, it was my job to lie there realllllly still while they imaged me to make sure I was in the exact spot I was supposed to be in. and then treatment begins. After several treatments, you will probably start to memorize the exact movements and sounds that the machine makes, so you can gauge how much longer you have left during treatment. And for me, this made treatment pass by more quickly.
Each facility is different, so your treatment may or may not follow this same process but some elements will for sure be the same. Most of the time each treatment appointment will last generally the same amount of time and can also be scheduled around the same time of day each day. Your doctor will go over these details with you on your first day or before.
During my treatment, I kept a weekly journal on how things were going so that 1) my friends and family stayed updated and 2) to hopefully provide a resource for those facing treatment themselves or those who know someone who is.
Undertreat Visits and Follow-ups
Undertreat visits are the quick visits you will have with your radiation oncologist while you are under treatment. At UAB, I was seen by my RadOnc once a week for the 6 weeks I was having treatment. It was mainly for her to check and make sure all was going well and my symptoms/side effects were being managed. Things like weight, mobility, and general well-being will be looked at. Undertreats are typically on the same day each week and happen immediately following your treatment for the day.
Follow-ups are the appointments that you will go to after treatment is complete. Sometimes these appointments are accompanied by scans (MRIs or CTs) and sometimes they stand alone to check on your progress in healing and recovering. Your radiation oncologist might ask you questions about symptoms, skin and muscle tightness, and general mobility, and they also might ask you to perform simple tasks or movements depending on what your primary disease site was and where you were treated.
Other Info
Each person will obviously have a different experience with each of these phases of the journey. And you will find that some phases are easier than others whether that is physically, mentally, or emotionally. For more information, follow the links below:
Questions to ask your doctor (Before, during, and after treatment)
Radiation Treatment: Who’s on your care team?

It’s not surprising that a lot goes on behind the scenes of radiation therapy, and it’s definitely not surprising to you that there are many different people that have a hand in your care. With all the people that you see during your visits, there are just as many behind the scenes folks that have a role in what will happen from consult to continued follow-ups.
PLANNING TEAM
Dosimetrists
Dosimetrists are some of the first people to look at your case after your pathologist and doctor. These are the people that are eyeballs deep in graphs, formulas, and scans making sure that your treatment is planned correctly so that your treatment will target the most effective areas. Dosimetrists carefully calculate the dose of radiation you will receive and the daily machine settings/parameters.
Once they finish their work on your case, they pass the plan back to your radiation oncologist for their approval, and then your plan is ready to be put into action.
Radiation Physicists
It may sound strange for a physicist to be a part of your radiation oncology team, but they serve a very important role in the precision and accuracy of your treatment. Our physicists keep our radiation treatment machines properly calibrated each and every day by taking precise measurements of the radiation equipment output. They also ensure that the machines are delivering the precise dose of radiation during each and every treatment which is particularly important for patients that undergo daily radiation treatment.
TREATMENT TEAM
Certified Medical Assistants (CMAs)
CMAs are not a part of every care team but larger facilities tend to have someone in this role to help with patient flow. CMAs are the people on your care team that may perform duties similar to a nurse. They might take your vitals, ask you a variety of questions regarding your current and recent status, and get your ready to see the doctor.
Nurses
Your radiation therapy nurse is a registered nurse whose main job is to implement the plan of care your radiation oncologist has prescribed for you. Your nurse will be the one to administer medications and monitor any possible side effects or adverse reactions that you may experience during or after radiation treatment.
Radiation Therapists
You will see your radiation therapist every single day of your treatment. Your therapist will walk you to your treatment machine, get you setup in place, and make sure you are comfortable before leaving the room. But where are they going?
While you are on the treatment table, your radiation therapists are stationed nearby so they can monitor you and operate the machines. In many cases, they are taking quick images of your placement to make sure you are in the correct position so that the radiation will hit the correct spot, and they are also controlling the radiation. If anything were to happen mid-treatment, they can/will stop the machine and get to you as quickly as they can to make sure everything is ok. Once your treatment is complete, they will help you off the table and escort you back to the dressing/waiting areas.
In my experience, these people are angels (but don’t tell anyone else I said that.) My therapist talked to me, checked on me, and went above and beyond what they had to do to make sure I had a decent experience in the midst of a mess.
Radiation Oncologists (& Residents)
Radiation Oncologists are crucial to your care. They are the medical minds that oversee every bit of your radiation oncology care. They review your pathology, pinpoint the exact location(s) of the tumor or lesions on various scans, plan your dose of radiation and how many treatments you will have, manage your symptoms throughout your treatment, and do their best to ensure you get the best treatment and care you can, whether that’s curative or palliative treatment.
Your Radiation Oncologist should be skilled and very knowledgeable about the typical side effects, prognosis, standards of care, and research opportunities that might be available. They are the ones that you should direct your questions to at your visit, but it is important to understand that there are some questions that your doctor simply isn’t able to answer.
At many facilities, residents are a part of the radiation oncology team as well. Residents may visit your room first and ask you questions during an exam or they may enter the exam room with your regular physician. Throughout their residency, residents are often times observing and absorbing as much information about each patient and the appropriate care as they can as they move closer to graduation. You also might notice that depending how much time passes between your visits, there may be a different resident present for your visit than before. Residents rotate doctors so that they have a wide variety of experience by the time they finish their residency.
THE REST OF THE TEAM
Research Study Coordinators
Depending on whether or not your doctor recommends that you participate in a clinical trial, you may or may not interact with a study coordinator. These folks are the experts in the department on the clinical studies open in that practice, and will make sure each aspect of the study elements outside of standard of care treatment is taken care of. These will also be the people most likley to explain the study to you and call and check on you for follow-ups. These follow-ups may be in person at your regular visits or they may be a telephone call to see how you’re doing.
Social Services
Lastly, social workers are there specifically for you! Their purpose is to make sure you are taken care of and provide you with the tools to deal with emotional burdens you may experience and/or help with decision making strategies for your care. Social workers also typically have the ability to assist with more concrete needs including housing, transportation, finances, hopsice or home care, and other supportive resources.